Background
Acute coronary syndrome (ACS) refers to a spectrum of clinical conditions caused by acute myocardial ischemia. It is most commonly due to the disruption (rupture or erosion) of an unstable atherosclerotic plaque in a coronary artery, leading to partial or complete thrombosis, and reduced myocardial blood flow.
Classification/Types
ACS is primarily classified based on electrocardiographic changes and cardiac biomarker levels into the following categories:
1. Unstable Angina (UA):
- Ischemia without infarction
- ECG: May show ST depression or T-wave inversion;
- no persistent ST elevation
- Cardiac biomarkers (e.g., troponin): Normal
- Pathophysiology: Partial or transient occlusion
- without myocardial necrosis
2. Non–ST Elevation Myocardial Infarction (NSTEMI):
- Ischemia with infarction (subendocardial)
- ECG: May show ST depression or T-wave inversion
- Cardiac biomarkers: Elevated troponin indicating
- myocardial necrosis
- Pathophysiology: Partial or transient occlusion
- causing subendocardial infarction
3. ST-Elevation Myocardial Infarction (STEMI):
- Transmural infarction due to complete arterial occlusion
- ECG: Persistent ST-segment elevation in contiguous
- leads or new left bundle branch block (LBBB)
- Cardiac biomarkers: Elevated troponin
- Pathophysiology: Complete and prolonged occlusion of a
- coronary artery
Pathophysiology
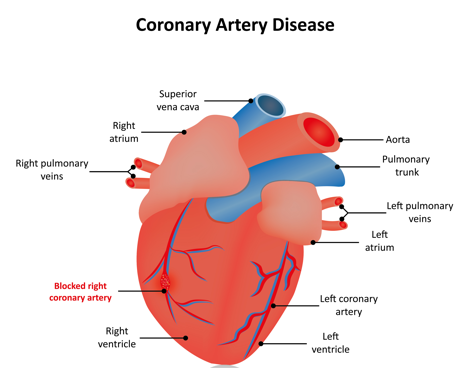
Acute Coronary Syndrome (ACS) is primarily triggered by a sudden reduction in blood flow to the heart, most commonly due to the rupture or erosion of an atherosclerotic plaque in a coronary artery.
The disrupted plaque exposes subendothelial matrix, leading to platelet adhesion, activation, and aggregation. This initiates the formation of a thrombus within the coronary artery.
If the thrombus fully occludes the vessel, it results in ST-elevation myocardial infarction (STEMI). If the occlusion is partial or transient, it leads to non–ST elevation ACS, which includes NSTEMI and unstable angina.
The reduced coronary perfusion causes an imbalance between myocardial oxygen supply and demand, resulting in ischemia. If ischemia is prolonged, it can lead to irreversible myocardial cell injury and necrosis (infarction).
An accompanying inflammatory response, oxidative stress, and neurohormonal activation may worsen myocardial damage and contribute to complications such as arrhythmias, heart failure, or sudden cardiac death.
Clinical Presentation
History (Symptoms)
Patients typically present with chest pain (angina) described as pressure, tightness, or heaviness in the retrosternal area. It may radiate to the left arm, neck, jaw, or back, and usually lasts >20 minutes.
- Pain is often not relieved by rest or sublingual nitroglycerin in ACS (especially NSTEMI/STEMI).
- Associated symptoms include dyspnea, nausea, vomiting, diaphoresis, palpitations, and lightheadedness.
- Atypical presentations (especially in elderly, diabetics, and women) include dyspnea without pain, epigastric discomfort, or fatigue.
Physical Exam (Signs)
Vital Signs:
- Heart rate (HR): Tachycardia due to sympathetic activation or bradycardia in inferior wall MI (due to vagal stimulation or AV block)
- Blood pressure (BP): May be hypertensive (due to pain/stress or history of hypertension) or hypotensive in cardiogenic shock or right ventricular (RV) infarct
- Oxygen saturation (SO2): May be decreased in extensive myocardial infarction (MI) or pulmonary congestion
- Temperature: Usually normal but can rise in late post-infarction stages due to inflammation
Cardiovascular:
- S3 gallop indicates left ventricular dysfunction
- New murmurs, such as a holosystolic murmur at the apex, may suggest papillary muscle rupture (acute mitral regurgitation)
- Irregular rhythms may point to arrhythmias like atrial fibrillation or premature ventricular contractions (PVCs)
Respiratory:
- Bibasilar crackles may indicate pulmonary edema from left-sided heart failure
- Tachypnea can be a compensatory response to hypoxia or acidosis
Peripheral Vascular:
- Cool extremities, delayed capillary refill, and weak pulses may be signs of cardiogenic shock
- Jugular venous distension (JVD) may be seen in RV infarction or biventricular failure
Neurological:
- Altered mental status may occur due to hypoperfusion to the brain in shock states.
Diagnostic Testing
Initial Tests
I) 12-lead ECG (immediately):
It is the best initial test to evaluate ACS.
- STEMI: ST elevations ≥1 mm in 2 or more contiguous leads
- NSTEMI/UA: ST depressions, T-wave inversions, or nonspecific changes
MI Location, Artery Involved, and ECG Leads
MI Location | Coronary Artery Involved | ECG Leads with ST Elevation |
Anteroseptal | Left Anterior Descending (LAD) | V1–V2 |
Anteroapical | Distal LAD | V3–V4 |
Anterolateral Wall | Left Circumflex (LCX) or LAD | V5–V6 |
Lateral Inferior Wall | LCX Right Coronary Artery (RCA) | I, aVL II, III, aVF |
Posterior Wall | Posterior Descending Artery (PDA) | V7–V9 (posterior leads) |
Right Ventricle | RCA (proximal) | V4R (right-sided ECG) |
Extensive Anterior | Left Main or Proximal LAD | V1–V6, I, aVL |
II) Cardiac Biomarkers/Enzymes:
- CK-MB, Troponins (I/T) : Elevation = myocardial injury; used to distinguish NSTEMI from UA
- Elevated in STEMI and NSTEMI
- Unstable Angina: Normal cardiac enzymes
- Recheck every 3–6 hours
Cardiac Enzymes in MI: Onset, Peak, and Duration
Biomarker | Time to Rise | Peak | Return to Normal | Clinical Notes |
Troponin I/T | 3–6 hours | 12–24 hours | 7–10 days (I), 10–14 days (T) | Most specific and sensitive for MI. Elevated longer — useful for late presentation.
|
CK-MB | 3–6 hours | 12–24 hours | 2–3 days | Useful for detecting reinfarction after initial MI due to shorter half-life.
|
Myoglobin | 1–2 hours | 6–9 hours | 24 hours | Earliest to rise, but least specific (also elevated in muscle injury).
|
LDH (LDH-1) | 12–24 hours | 2–3 days | 7–10 days | Historically used; rarely used now due to poor specificity. |
Additional Lab Tests
- CBC, CMP, lipid panel, glucose, coagulation panel
- BNP if heart failure is suspected
- ABG if hypoxia present
- Urine drug screen in young patients with unclear etiology
Imaging
I) Coronary angiography:
It is the most accurate test to diagnose CAD. Gold standard for evaluating coronary anatomy.
It is used to detect the anatomic location of coronary artery disease. Surgically correctable disease generally begins with 70% or greater stenosis.
II) Chest X-ray: Rule out pneumonia, aortic dissection, pneumothorax
III) Echocardiography: Evaluate wall motion abnormalities and ejection fraction. Decreased wall motion is seen in CAD. Ischemia causes reversible wall motion. Infarction is irreversible/fixed.
Types of ACS
Type | ECG Changes | Troponin | Occlusion |
UA | Normal/ST↓/T↓ | Normal | Partial/Transient |
NSTEMI | ST↓/T↓/Non-specific | Elevated | Partial/Prolonged |
STEMI | ST↑ in 2+ leads | Elevated | Complete coronary occlusion |
Differential Diagnosis of Chest Pain
Cardiac
- Pericarditis: Pleuritic pain, pericardial friction rub, diffuse ST elevation
- Aortic dissection: Tearing pain radiating to back, pulse deficits
- Heart failure exacerbation: Dyspnea, orthopnea, edema
Pulmonary
- Pulmonary embolism: Sudden dyspnea, pleuritic chest pain, tachycardia
- Pneumothorax: Unilateral decreased breath sounds, hyperresonance
- Pneumonia: Fever, cough, focal consolidation
Gastrointestinal (GI)
- GERD: Burning sensation, worsens when lying flat
- Esophageal spasm: Mimics angina, unresponsive to nitroglycerin
- Peptic ulcer disease: Epigastric pain, relief with antacids
Musculoskeletal (MSK)
- Costochondritis: Reproducible chest wall tenderness
Muscle strain: Focal pain, history of exertion
Treatment
Current ACC/AHA and ESC guidelines (2021–2024 updates) have refined the initial management of Acute Coronary Syndrome (ACS). The emphasis now is on evidence-based pharmacotherapy, rapid reperfusion, and risk stratification.
| Step | Intervention | Notes |
|---|---|---|
| A | Aspirin | 325 mg PO chewed immediately (loading dose 162–325 mg); reduces mortality. Continue 81 mg daily. |
| P | P2Y12 Inhibitor (Clopidogrel, Ticagrelor, Prasugrel) | Initiate dual antiplatelet therapy (DAPT) unless contraindicated. Choice depends on PCI vs. fibrinolysis strategy. |
| A | Anticoagulation (UFH, LMWH, or bivalirudin) | Prevents thrombus propagation. UFH common in PCI; LMWH (enoxaparin) in NSTEMI. |
| S | Statins (high-intensity) | Atorvastatin 80 mg or rosuvastatin 20–40 mg; stabilize plaque, reduce recurrent events. Start early. |
| B | Beta-blockers (e.g., metoprolol) | Start within 24h unless contraindicated (hypotension, bradycardia, heart block, decompensated HF, cocaine use). Reduce arrhythmia and mortality. |
| A | ACE inhibitors / ARBs / ARNi | Begin within 24h if LVEF <40%, diabetes, HTN, CKD, or anterior MI. Proven mortality benefit. |
| N | Nitrates | For chest pain (avoid in hypotension, RV infarction, PDE-5 inhibitor use). Sublingual first; IV if persistent. |
| O | Oxygen | Only if SpO₂ <90%, respiratory distress, or shock. Routine O₂ is not beneficial. |
| M | Morphine | Reserved for refractory pain/anxiety after nitrates. Use cautiously (may mask symptoms, ↑mortality in some studies). |
Note: In inferior wall MI (ie, RV infarction), avoid nitrates and diuretics due to risk of severe hypotension (preload dependent). IV fluids are best administered to improve hemodynamics by increasing preload.
Reperfusion Therapy (Door-to-balloon time for STEMI)
- Primary Percutaneous Coronary Intervention (PCI) within 90 minutes of first medical contact (gold standard)
- Thrombolytics (e.g., alteplase) if PCI is unavailable within 120 minutes
- Contraindications include active bleeding, recent stroke, or severe hypertension
Adjuncts
Glycoprotein IIb/IIIa inhibitors (e.g., abciximab) in selected high-risk PCI patients.
Aldosterone antagonists (eplerenone, spironolactone) if EF ≤40% + diabetes or HF, post-MI.
Proton pump inhibitors if high bleeding risk on DAPT.
Types of Stents in PCI
Stent Type | Description | Common Uses |
Bare-Metal Stent (BMS) | A simple metal scaffold without drug coating | Rarely used now; considered when short DAPT is needed |
Drug-Eluting Stent (DES) | Coated with antiproliferative drugs (e.g., sirolimus, everolimus, zotarolimus) | First-line for most cases; lowers restenosis risk |
Indications for Coronary Artery Bypass Graft (CABG)
- Left main coronary artery disease
- Multi-vessel disease (especially in diabetics or reduced EF)
- Failed PCI
- Severe proximal LAD stenosis with complex anatomy
Long-Term Treatment and Mortality-Reducing Therapies
Medication | Mortality Benefit | Notes |
Aspirin | Yes | Lifelong; cornerstone of therapy |
Beta-blockers | Yes | Decrease myocardial oxygen demand, reduce arrhythmias |
ACE inhibitors / ARBs | Yes | Prevent remodeling; especially in diabetics, HTN, or low EF |
Statins | Yes | Stabilize plaques, lower LDL |
Aldosterone antagonists (e.g., spironolactone) | Yes | In patients with EF <40% and HF or DM, after MI |
DAPT (aspirin + P2Y12 inhibitor) | Yes | Continue for 12 months post-MI/PCI |
Post-MI Complications
I) Immediate (0–24 hours) Arrhythmias
- Types: Ventricular fibrillation (VF), ventricular tachycardia (VT), atrial fibrillation, AV block
- Pathophysiology: Electrical instability due to ischemic myocardium
- Clues: Sudden cardiac arrest, palpitations, syncope, bradycardia
- High risk: Anterior MI and inferior MI (AV nodal ischemia)
II) Early (1–3 Days)
Pericarditis (early)
- Pathophysiology: Inflammatory response of pericardium over infarcted myocardium
- Presentation: Sharp, pleuritic chest pain relieved by leaning forward; pericardial friction rub; diffuse ST elevation without reciprocal changes
- Treatment: Aspirin
III) Subacute (3–7 Days)
1. Papillary Muscle Rupture
- Pathophysiology: Infarction → necrosis → rupture, especially of posteromedial muscle (RCA-dependent)
- Clues: Acute severe mitral regurgitation, flash pulmonary edema, hypotension, new loud holosystolic murmur at apex
- Seen in: Inferior MI
2. Interventricular Septal Rupture
- Pathophysiology: Full-thickness necrosis of septum leads to left-to-right shunt
- Clues: Sudden heart failure, cardiogenic shock, harsh holosystolic murmur at LSB, oxygen step-up in RV
3. Free Wall Rupture
- Pathophysiology: Full-thickness LV rupture leads to hemopericardium → tamponade → PEA
- Clues: Sudden death, pulseless electrical activity, hypotension, distended neck veins, muffled heart sounds (Beck’s triad)
- Seen in: Elderly, female, first MI, no prior infarct/scar
IV) Late (1–2 Weeks)
Mural Thrombus
- Pathophysiology: Akinesis + endocardial damage → thrombus formation in LV
- Clues: Asymptomatic or systemic embolism (stroke, limb ischemia)
- Dx: Echocardiogram
- Tx: Anticoagulation (e.g., warfarin)
V) Chronic (2 Weeks to Months)
1. Left Ventricular Aneurysm
- Pathophysiology: Scarred, thinned myocardium balloons outward during systole
- Clues: Persistent ST elevations on ECG, HF symptoms, embolic strokes, ventricular arrhythmias
2. Dressler Syndrome (Post-MI Syndrome)
- Pathophysiology: Autoimmune pericarditis triggered by myocardial antigens
- Clues: Fever, pleuritic chest pain, pericardial effusion, elevated ESR
- Tx: NSAIDs (ibuprofen) ± colchicine; avoid anticoagulation due to bleeding risk with effusion
Patient Education
Education
Smoking cessation: Strongest modifiable risk factor
Diet: Low-sodium, low-saturated fat (DASH or Mediterranean)
Exercise: At least 150 min/week of moderate-intensity aerobic activity
Medication adherence: Crucial for secondary prevention
Vaccines
Influenza and pneumococcal vaccines recommended in all patients with CAD
Follow-Up
Cardiology follow-up within 1 week post-discharge
Monitor BP, lipids, renal function
Refer to cardiac rehabilitation for structured recovery
Assess for depression post-MI
Erectile dysfunction post-MI is mostly due to anxiety. Beta-blockers are a common cause of ED. Do not combine nitrates with sildenafil due to the risk of profound hypotension.
Stay on top of medicine. Get connected. Crush the boards.
HMD is a beacon of medical education, committed to forging a global network of physicians, medical students, and allied healthcare professionals.