Cardiology > Acute Decompensated Heart Failure
Acute Decompensated Heart Failure
Background
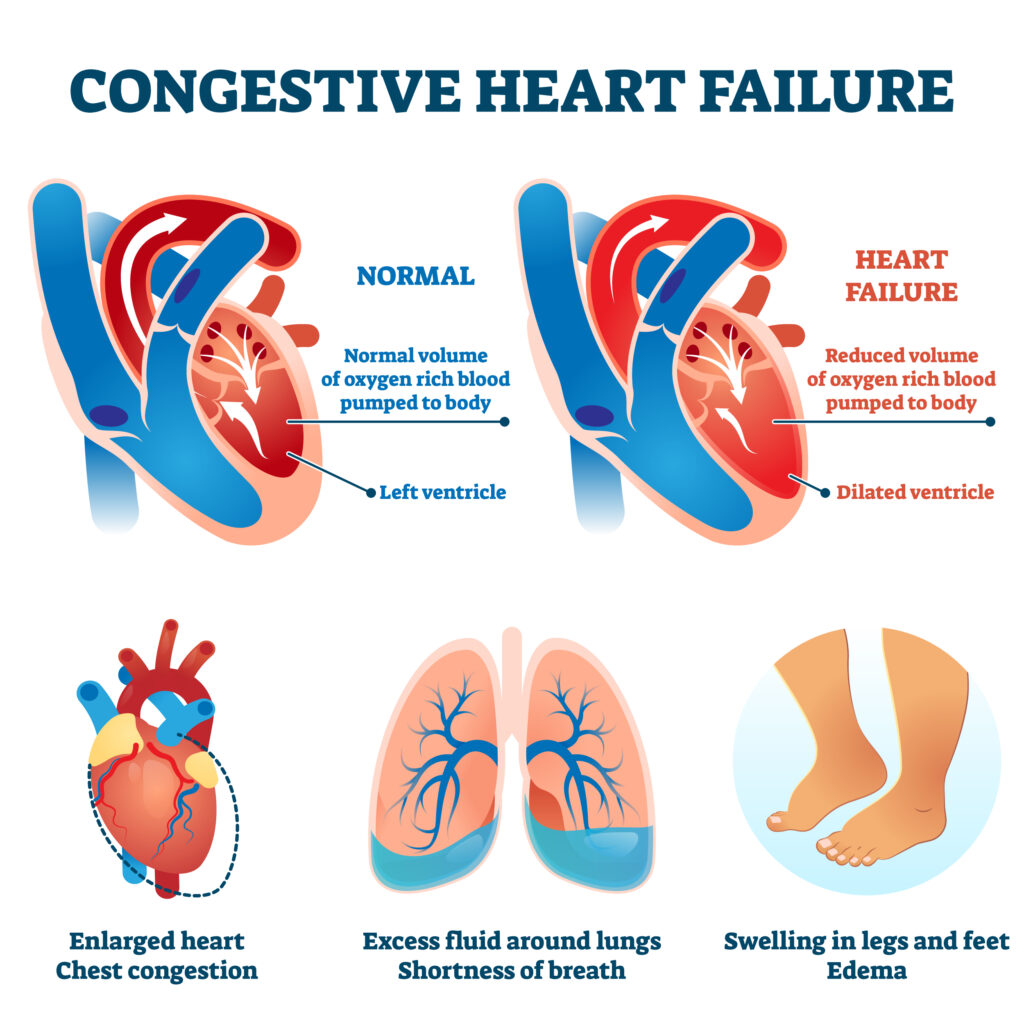
Acute Decompensated Heart Failure (ADHF) is a sudden or gradual worsening of heart failure signs and symptoms, often leading to hospitalization. It reflects volume overload, hypoperfusion, or both, resulting from impaired ventricular filling or ejection. ADHF may occur in patients with chronic heart failure (acute-on-chronic) or as a new presentation (de novo heart failure).
II) Classification/Types
- De novo heart failure: First-time presentation of heart failure, usually from acute myocardial injury or hypertensive crisis.
- Acute-on-chronic heart failure: Worsening symptoms in a patient with known heart failure due to fluid overload, ischemia, arrhythmias, or nonadherence.
- Wet vs. dry (volume status) and warm vs. cold (perfusion status) are commonly used clinical profiles to guide management:
I) Warm and wet: Adequate perfusion with
congestion (most common)
II) Cold and wet: Hypoperfusion with congestion
(worst prognosis)
III) Warm and dry: Compensated state
IV) Cold and dry: Hypoperfusion without volume
overload (rare)
III) Epidemiology
- Sex: Slightly more common in men, but women tend to live longer with HF and may present more often with preserved EF.
- Age: Most patients are over 65 years; incidence increases with age.
- Race/Region: Higher prevalence among African Americans; associated with increased hospital readmissions.
- Social Status: More common in low-income populations due to limited access to medical care, higher rates of hypertension and diabetes.
Etiology
I) Causes:
- Nonadherence to medications or diet (most common)
- Uncontrolled hypertension
- Myocardial ischemia/infarction
- Arrhythmias (e.g., atrial fibrillation with rapid ventricular response)
- Infections (e.g., pneumonia, sepsis)
- Valvular heart disease (e.g., aortic stenosis)
- Renal failure or volume overload from iatrogenic IV fluids
- Pulmonary embolism
- Anemia or thyroid dysfunction
II) Risk Factors
- Known heart failure (reduced or preserved EF)
- Coronary artery disease
- Hypertension
- Diabetes mellitus
- Chronic kidney disease
- High salt or fluid intake
- Medication nonadherence
- Alcohol or cocaine use
Clinical Presentation
I) History (Symptoms)
- Dyspnea, especially on exertion or when lying flat (orthopnea)
- Paroxysmal nocturnal dyspnea (PND)
- Fatigue and decreased exercise tolerance
- Cough (often productive of frothy sputum)
- Rapid weight gain
- Abdominal discomfort, bloating
- Reduced urine output (oliguria)
- Symptoms of hypoperfusion: dizziness, cold extremities, confusion
II) Physical Exam / Signs
Vital Signs:
- Pulse : Tachypnea, tachycardia
- Pulse Oximetry: Hypoxia
- Blood Pressure: Hypertension or hypotension depending on stage
- Temperature: Fever if underlying infection
Cardiovascular:
- Elevated jugular venous pressure (JVP)
- S3 gallop (volume overload)
- Displaced or diffuse apical impulse
- New or changed murmur
Pulmonary:
- Bibasilar crackles (rales)
- Wheezing (“cardiac asthma”)
- Dullness to percussion (pleural effusions)
Abdomen:
- Hepatomegaly
- Hepatojugular reflux
- Ascites
Peripheral:
- Pitting peripheral edema
- Cool extremities with poor capillary refill in severe cases
Differential Diagnosis (DDx)
- COPD or asthma exacerbation
- Pneumonia
- Pulmonary embolism
- Acute coronary syndrome
- Cirrhosis with ascites
- Nephrotic syndrome
- Pericardial tamponade
Diagnostic Tests
Initial Tests:
- Echocardiogram (Transthoracic):
- Ejection fraction (reduced or preserved)
- Wall motion abnormalities (ischemia)
- Valvular abnormalities
- Echocardiogram (Transthoracic):
- Electrocardiogram (ECG):
- May show ischemia, infarction, arrhythmia (e.g., atrial fibrillation)
- Electrocardiogram (ECG):
- Chest X-ray:
- Cardiomegaly
- Pulmonary venous congestion
- Interstitial edema, Kerley B lines
- Pleural effusions
- Chest X-ray:
- BNP or NT-proBNP:
- Elevated in heart failure; helps differentiate from pulmonary causes of dyspnea
- BNP or NT-proBNP:
- Cardiac Enzymes (CK-MB, Troponins):
- Elevated in myocardial infarction or strain
- Cardiac Enzymes (CK-MB, Troponins):
- Basic labs:
- CMP: electrolyte disturbances, renal dysfunction
- CBC: anemia or leukocytosis
- TSH: screen for thyroid dysfunction
- ABG: hypoxia, hypercapnia
- LFTs: may show congestive hepatopathy
- Basic labs:
Treatment
I) Initial Stabilization:
- Oxygen therapy: if hypoxic
- Noninvasive ventilation (CPAP/BiPAP): for respiratory distress
- IV access and cardiac monitoring
- Address reversible causes (e.g., MI, arrhythmias, infections)
II) Volume Overload (“Wet”) Management:
- Loop diuretics (e.g., IV furosemide): first-line for symptom relief
- Monitor for hypotension, renal function, electrolytes
- Vasodilators (if hypertensive): IV nitroglycerin or nitroprusside
III) Hypoperfusion (“Cold”) Management:
- Inotropes (e.g., dobutamine, milrinone): for low-output states
Use with caution; may increase mortality with
long-term use
- Vasopressors (e.g., norepinephrine): in shock or profound hypotension
IV) Additional Therapies:
- SGLT2 inhibitors, ACE inhibitors/ARBs, beta-blockers, MRA (in HFrEF): resume or initiate once patient stabilizes
- Ultrafiltration: if diuretic-resistant volume overload
Consults
- Cardiology: for unclear etiology or persistent symptoms
- Nephrology: if renal function declines or ultrafiltration needed
- Pharmacy: for medication optimization
- Social work/case management: for discharge planning, medication access
- Palliative care: for advanced HF or frequent hospitalizations
Patient Education
- Daily weight monitoring at home
- Low-sodium diet and fluid restriction as advised
- Medication adherence education
- Smoking and alcohol cessation
- Avoid NSAIDs (they worsen heart failure)
- Annual influenza and pneumococcal vaccines
- COVID-19 vaccination per guidelines
Follow-Up
- Reassess volume status, weight, renal function, and symptoms
- Optimize guideline-directed medical therapy (GDMT)
- Educate on early signs of decompensation
- Follow up within 7 days of discharge to reduce readmission
- Regular cardiology follow-up for titration of medications
Stay on top of medicine. Get connected. Crush the boards.
HMD is a beacon of medical education, committed to forging a global network of physicians, medical students, and allied healthcare professionals.