Cardiology > Heart Failure (HF)
Heart Failure (HF)
Background
Heart failure (HF) is a clinical syndrome characterized by the heart’s inability to pump sufficient blood to meet the metabolic demands of the body. It results from structural or functional cardiac disorders impairing ventricular filling or ejection of blood.
Classification
Heart failure is classified based on several factors:
A) Based on Ejection Fraction (EF):
- HFrEF (Heart Failure with reduced EF): EF < 40%
- HFpEF (Heart Failure with preserved EF): EF ≥ 50%
- HFmrEF (mildly reduced EF): EF 41–49%
Type | EF (%) | Pathophysiology | Common Causes |
HFrEF (reduced EF) | <40% | Systolic dysfunction: impaired contraction of LV | CAD, MI, dilated cardiomyopathy |
HFmrEF (mildly reduced EF) |
41–49% | Intermediate phenotype; partly systolic and partly diastolic | Mixed causes |
HFpEF (preserved EF) |
≥50% | Diastolic dysfunction: impaired relaxation and filling | HTN, aging, obesity, diabetes, HCM |
HFrEF is also known as systolic dysfunction.
HFpEF is similarly referred to as diastolic dysfunction.
B) Based on Anatomy: Left-Sided vs Right-Sided Heart Failure
I ) Left-Sided Heart Failure (LHF)
- Inability of the left ventricle to pump blood effectively to the systemic circulation.
Causes:
- Ischemic heart disease (MI, CAD)
- Hypertension
- Aortic stenosis
- Mitral regurgitation
- Dilated or hypertrophic cardiomyopathy
II) Right-Sided Heart Failure (RHF)
Inability of the right ventricle to pump blood effectively into the pulmonary circulation.
Causes:
- Left-sided heart failure (most common)
- Pulmonary hypertension
- COPD → cor pulmonale
- Pulmonary embolism
- Tricuspid or pulmonary valve disease
- Right ventricular infarct (RMI)
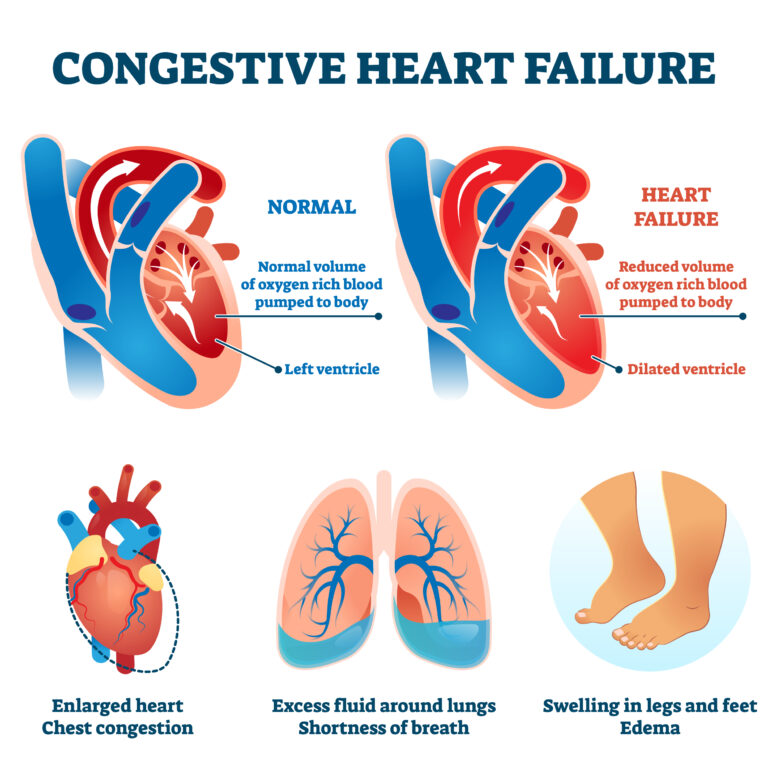
III) Congestive Heart Failure (CHF)
- Is a term used when both sides are failing
- Often starts as LHF → leads to RHF due to pulmonary pressure overload
- Presents with combined pulmonary and systemic congestion
C) Based on Timing of Onset:
- Acute vs. Chronic: Acute HF presents suddenly, while chronic HF develops over time with periods of stability and exacerbation.
- Acute Decompensated Heart Failure (ADHF)
- Acute Decompensated Heart Failure is a sudden or gradual worsening of heart failure symptoms, usually in a patient with pre-existing chronic HF. It is a medical emergency and a leading cause of hospitalization in older adults.
- ADHF = acute worsening of cardiac function → volume overload, poor perfusion, or both
May present as:
- ADHF = acute worsening of cardiac function → volume overload, poor perfusion, or both
Worsening of chronic HF (most common)
New-onset (“de novo”) heart failure (e.g., from MI or
hypertensive crisis)
D) High-Output Heart Failure
High-output heart failure is a less common form of heart failure where cardiac output is elevated, but still inadequate to meet the body’s metabolic demands. Unlike typical low-output heart failure, the problem isn’t weak pumping — it’s the body’s excessive demand or abnormally low systemic vascular resistance.
High-output heart failure occurs when the heart is pumping more than normal (> 8 L/min), yet the tissues remain hypoperfused due to:
- Low systemic vascular resistance, or
- Increased metabolic demand
The heart itself may be structurally normal or even hyperdynamic initially, but sustained overwork leads to eventual cardiac dysfunction.
Etiology
A) Causes of HFrEF (EF <40%)
Primary mechanism:
- Impaired contractility/systolic dysfunction
I) Ischemic causes (most common)
- Myocardial infarction (MI)
- Chronic coronary artery disease (CAD)
- Hibernating myocardium
II) Non-ischemic cardiomyopathies
- Dilated cardiomyopathy (idiopathic, familial/genetic)
- Toxic: Alcohol, cocaine, chemotherapy (e.g., doxorubicin, trastuzumab)
- Infectious: Viral myocarditis (e.g., Coxsackievirus, adenovirus)
- Peripartum cardiomyopathy
- Tachycardia-induced cardiomyopathy (e.g., from AF with RVR)
III) Pressure/volume overload
- Chronic hypertension
- Aortic or mitral regurgitation
- Severe aortic stenosis (late stages)
IV) Metabolic and systemic
- Thyroid dysfunction (especially hyperthyroidism)
- Nutritional (thiamine deficiency — wet beriberi)
- Iron overload (hemochromatosis)
V) Infiltrative/autoimmune
- Sarcoidosis
- Systemic lupus erythematosus (rare)
B) Causes of HFpEF (EF ≥50%)
Primary mechanism:
Impaired relaxation/diastolic dysfunction + ventricular stiffness
I) Common comorbid conditions
- Chronic hypertension (leads to LV hypertrophy)
- Aging (decreased compliance)
- Obesity (increased cardiac workload)
- Diabetes mellitus
- Coronary artery disease (ischemia without infarction)
II) Cardiomyopathies
- Hypertrophic cardiomyopathy
- Restrictive cardiomyopathy:
- Amyloidosis
- Hemochromatosis (early stage)
- Sarcoidosis
III) Valvular disease
- Aortic stenosis (early stages)
- Mitral stenosis
IV) Other
- Atrial fibrillation (impairs LV filling)
- High-output states (e.g., anemia, thyrotoxicosis — in vulnerable patients)
- Constrictive pericarditis
Right-Sided vs. Left-Sided Heart Failure
Feature | Left HF | Right HF |
Main cause | CAD, HTN | LHF, pulmonary disease |
Backup | Into lungs | Into systemic veins |
Symptoms | Dyspnea, orthopnea, fatigue | JVD, edema, ascites |
Key signs | Rales, S3, PND | Hepatomegaly, peripheral edema |
Triggers/Precipitating Causes of ADHF (“FAILURES”):
Mnemonic: FAILURES | Description
|
F – Forgot medications | Noncompliance with diuretics or HF meds
|
A – Arrhythmias | Atrial fibrillation, VT, bradyarrhythmias
|
I – Ischemia | Acute MI, unstable angina
|
L – Lifestyle | High salt/fluid intake, alcohol
|
U – Upregulation of CO | Infection, anemia, fever, thyrotoxicosis
|
R – Renal failure | Volume retention, worsening uremia
|
E – Embolism | PE causing acute RV strain
|
S –Stenosis/Structural | Valve disease (e.g., aortic stenosis), cardiomyopathies |
Common Causes of Right HF (Mnemonic: AV FISTULA)
Cause | Mechanism |
Anemia | ↓ Oxygen-carrying capacity → ↑ cardiac demand
|
Vitamin B1 deficiency (wet beriberi) | Vasodilation, impaired myocardial metabolism
|
Fistulas (arteriovenous) | Bypass capillaries → ↓ resistance → ↑ preload
|
Infection (sepsis) | Cytokine-induced vasodilation
|
Systemic vasodilation (e.g., cirrhosis) | ↓ SVR → ↑ cardiac output to maintain pressure |
Thyrotoxicosis | ↑ metabolic rate and sympathetic activity
|
Uremia | Toxins → vasodilation, anemia
|
Liver disease (esp. cirrhosis, hepatorenal syndrome) | Splanchnic vasodilation
|
Alcoholic wet beriberi | Thiamine deficiency-induced heart failure |
HF Risk Factors:
- Diabetes mellitus
- Smoking
- Obesity
- Chronic kidney disease
- Sleep apnea
- Advanced age
- Excessive alcohol use
- Family history of cardiomyopathy
Clinical Presentation
History (Symptoms)
- Exertional dyspnea and/or dyspnea at rest
- Orthopnea
- Acute pulmonary edema (PND, frothy sputum, wheezing)
- Chest pain/pressure and palpitations
- Fatigue and weakness
- Nocturia and oliguria
- Anorexia, weight loss, nausea
Physical Exam (Signs)
Vital Signs:
- Blood Pressure: Hypotension in advanced HF
- Pulse: Tachycardia due to sympathetic stimulation
– Weak, rapid, and thready pulse
- Respiratory Rate: Tachypnea from pulmonary edema
- O2 sat: Hypoxia in decompensated states
Cardiovascular:
- S3 gallop: Sign of volume overload and systolic dysfunction
- Displaced apical impulse: Suggests LV hypertrophy or dilation
- Jugular venous distention (JVD): Indicates elevated right-sided pressures
- Pulsus alternans: Alternating strong and weak pulse in advanced HF
Respiratory:
- Bibasilar crackles or rales: Pulmonary edema
- Wheezing (“cardiac asthma”)
- Pleural effusions: Often bilateral, right > left
Abdominal:
- Hepatomegaly and hepatojugular reflux: from hepatic congestion
- Ascites: Seen in severe right-sided HF
- Anasarca (generalized swelling)
Peripheral Vascular:
- Pitting edema in lower extremities
- Cool extremities in low output states
Neurological:
- Confusion, dizziness: Hypoperfusion in advanced cases
Differential Diagnosis
- COPD/Asthma exacerbation:
Wheezing, no orthopnea or edema
- Pneumonia:
Fever, consolidation on imaging
- Pulmonary embolism:
Pleuritic chest pain, sudden onset dyspnea
- CKD/Nephrotic syndrome:
Edema without dyspnea
- Liver cirrhosis:
Ascites, but no pulmonary signs
Diagnosing Heart Failure
Framingham Criteria:
Requires ≥2 major or 1 major + 2 minor criteria to diagnose heart failure:
Major:
- PND
- Neck vein distension
- Rales
- Cardiomegaly on CXR
- Pulmonary edema
- S3 gallop
- Weight loss ≥4.5 kg with treatment
Minor:
- Peripheral edema
- Night cough
- Dyspnea on exertion
- Hepatomegaly
- Pleural effusion
- Tachycardia
- Nocturnal dyspnea
Diagnostic Workup:
Initial Tests:
I) Echocardiogram (transthoracic):
- Is the best initial test to evaluate HF
- Most important tool for evaluating EF, chamber size, wall motion, valvular disease
- Classify HF as HFrEF or HFpEF
II) 12-lead ECG:
- May show arrhythmias, prior MI, LV hypertrophy
III) BNP or NT-proBNP:
- BNP = B-type natriuretic peptide; NT-proBNP = N-terminal proBNP (BNP precursor)
- Elevated in heart failure; helps distinguish from non-cardiac causes of dyspnea especially in atypical presentation
IV) Chest X-ray:
- Cardiomegaly, pulmonary vascular congestion, Kerley B lines, pleural effusions
Basic Lab Tests
|
|
| CBC May show anemia (common contributor to HF symptoms) |
|
CMP Hyponatremia (worsening prognosis), elevated BUN/creatinine, abnormal LFTs in hepatic congestion (congestive hepatomegaly, cardiac cirrhosis) |
| Lipid panel Assess atherosclerotic risk |
|
Thyroid panel Rule out hypo-/hyperthyroidism as reversible causes
|
| Cardiac Enzymes (CK-MB, Troponins) May be elevated in decompensation or coexisting ischemia |
|
Iron studies Screen for iron deficiency (common in HF, treatable) |
Other Imaging
- Cardiac MRI: For infiltrative or inflammatory cardiomyopathies
- Nuclear stress testing or coronary angiography: To assess for ischemic etiology
Management of Heart Failure
I) Acute Decompensated HF (ADHF)
Initial Treatment (“LMNOP”):
Step | Intervention | Notes |
L | Lasix (furosemide) | Loop diuretics for volume overload
|
M | Morphine (optional) | Anxiolytic and venodilator; use Cautiously
|
N | Nitrates (IV) | Reduce preload and pulmonary congestion (venodilator)
|
O | Oxygen | If hypoxic
|
P | Position | Upright position improves oxygenation |
II) Chronic HF Management (Mortality-Reducing Medications)
Medication | Mortality Benefit | Indication |
ACE inhibitors / ARBs (e.g., lisinopril, losartan)
| Yes | All patients with HFrEF unless contraindicated |
Beta-blockers (e.g., metoprolol succinate, carvedilol, bisoprolol)
| Yes | HFrEF; stabilize before initiation in ADHF |
Mineralocorticoid receptor antagonists (e.g., spironolactone, eplerenone)
| Yes | EF ≤ 35%, NYHA II–IV |
SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin)
| Yes | HFrEF or HFpEF; regardless of diabetes status |
ARNI (e.g., sacubitril/valsartan) | Yes | Replaces ACEi/ARB in HFrEF for superior outcomes
|
Hydralazine + isosorbide dinitrate | Yes (in Black patients) | NYHA III–IV despite optimal therapy or intolerance to ACEi/ARB
|
Ivabradine | No mortality reduction
| For HR >70 bpm despite max beta-blocker dose
|
Diuretics (e.g., furosemide, bumetanide) | Symptom relief only | For volume overload; monitor electrolytes |
Contraindications to Beta-Blockers:
- Acute decompensated HF
- Bradycardia or heart block
- Severe asthma/COPD exacerbation
- Cardiogenic shock
Device Therapy
I) Implantable Cardioverter Defibrillator (ICD):
- EF <35%, NYHA II–III despite optimal medical therapy
- An ICD (Implantable Cardioverter Defibrillator) is a device implanted in patients at high risk of sudden cardiac death (SCD) due to life-threatening ventricular arrhythmias, particularly in heart failure with reduced ejection fraction (HFrEF)
- Monitors heart rhythm continuously
Delivers:
- Pacing for bradycardia or minor arrhythmias
- Anti-tachycardia pacing (ATP) or
- Defibrillation shocks to terminate ventricular tachycardia/fibrillation
II) Cardiac Resynchronization Therapy (CRT):
- EF <35%, wide QRS (>150 ms), LBBB morphology
- Is a specialized pacing therapy used in heart failure with reduced ejection fraction (HFrEF) to improve ventricular synchrony, especially in patients with conduction delays (most commonly left bundle branch block – LBBB).
- Resynchronizes contraction of the left and right ventricles
- Improves:
- LV systolic function
- Cardiac output
- Symptoms and exercise tolerance
- Quality of life
- Reduces hospitalization and mortality
The New York Heart Association (NYHA) Classification
Is a functional system that categorizes heart failure (HF) based on the severity of symptoms and limitations to physical activity. It is widely used to assess baseline status, prognosis, and response to treatment.
Class I:
- No symptoms with ordinary physical activity.
- Example: Can climb stairs, walk uphill, or do moderate activity without fatigue or dyspnea.
Class II:
- Mild limitation of physical activity.
- Comfortable at rest, but ordinary activity (e.g., walking up 1 flight of stairs) causes fatigue, dyspnea, or palpitations.
Class III:
- Marked limitation of physical activity.
- Comfortable at rest, but less than ordinary activity (e.g., dressing, walking across the room) causes symptoms.
Class IV:
- Unable to carry out any physical activity without discomfort.
- Symptoms occur at rest (e.g., dyspnea, fatigue, palpitations). Any activity worsens discomfort.
Clinical Relevance
- Used for staging, treatment planning, and eligibility for advanced therapies (e.g., ICDs, transplant).
- Often correlates with quality of life and hospitalization risk.
- Can change over time depending on response to therapy.
Consults
- Cardiology: For advanced HF, device evaluation, or unclear etiology
- Electrophysiology: For ICD or CRT candidacy
- Nephrology: If renal dysfunction limits diuretic use or electrolyte control
- Palliative care: For refractory symptoms or advanced disease
Patient Education
- Daily weight monitoring: Report if gain >2–3 lbs in 1 day or >5 lbs in a week
- Recognize early signs of decompensation: increased dyspnea, edema, fatigue, orthopnea
Adhere to:
- Low-sodium diet (<2 g/day)
- Fluid restriction (<2 L/day if volume overloaded)
- Maintain physical activity as tolerated (encourage cardiac rehab if eligible)
- Emphasize smoking cessation and limit alcohol intake
- Take all medications as prescribed; do not stop beta-blockers or ACEi abruptly
- Keep all follow-up appointments for labs, imaging, and clinic visits
- Encourage caregivers to be involved in monitoring symptoms and adherence
Screen for and manage:
- Depression or cognitive decline (common in chronic HF)
- Sleep apnea (especially in HFpEF or refractory HFrEF)
- Iron deficiency (common even without anemia; IV iron improves symptoms)
- Thyroid dysfunction (both hypo- and hyperthyroidism can worsen HF)
- Diabetes and lipid control (optimize comorbidity management)
- Arrhythmias, especially atrial fibrillation or bradyarrhythmias
- Frailty or sarcopenia, particularly in elderly HFpEF patients
Vaccinations before discharge:
- Influenza vaccine annually
- Pneumococcal vaccines:
- PCV20 (or PCV15 + PPSV23 as alternative per CDC guidelines)
- COVID-19 vaccination and boosters
- Consider Tdap/Td if not up to date
Follow-Up
- Reassess EF after 3–6 months of optimal therapy
- Monitor weight, blood pressure, renal function, electrolytes regularly
- Educate on fluid (<2 L/day) and sodium (<2 g/day) restrictions
- Refer to cardiac rehab if stable
- Assess for medication side effects and adherence
Stay on top of medicine. Get connected. Crush the boards.
HMD is a beacon of medical education, committed to forging a global network of physicians, medical students, and allied healthcare professionals.