Cardiology > High Output Heart Failure
High Output Heart Failure
Background
High Output Heart Failure (HOHF) is a rare clinical syndrome where cardiac output is elevated (typically >8 L/min) due to increased metabolic demands or peripheral vasodilation, yet the heart still fails to meet systemic requirements. Despite the elevated cardiac output, patients develop typical heart failure symptoms due to circulatory overload and neurohormonal activation.
II) Classification/Types
Primary HOHF – Caused by intrinsic conditions that increase metabolic demand or reduce systemic vascular resistance.
Secondary HOHF – Occurs in preexisting cardiac disease (e.g., HFrEF) exacerbated by high-output states.
III) Epidemiology
- Sex: Affects both genders equally, depending on the underlying etiology.
- Age: Most often seen in adults, but can occur in children (e.g., AV malformations).
- Region: Prevalence depends on endemic diseases (e.g., thiamine deficiency in developing countries).
- Risk groups: Patients with chronic illnesses (e.g., cirrhosis, severe anemia, thyrotoxicosis).
Etiology
I) Causes
Anemia – Reduced oxygen-carrying capacity → increased cardiac output.
Thyrotoxicosis – Increases basal metabolic rate and HR/contractility.
Arteriovenous (AV) Fistulas – Bypass resistance vessels, increasing preload.
Beriberi (Thiamine deficiency) – Impairs myocardial energy utilization.
Paget’s disease of bone – Increased vascularity raises cardiac workload.
Cirrhosis – Splanchnic vasodilation leads to reduced SVR and hyperdynamic state.
Sepsis – Inflammatory vasodilation and increased tissue demand.
Obesity – Elevated metabolic demands and increased blood volume.
Pregnancy – Physiological high-output state may decompensate if cardiac reserve is limited.
II) Risk Factors
Chronic anemia
Hyperthyroidism
AV malformations (e.g., dialysis fistulas)
Nutritional deficiencies (especially B1)
Liver disease
Chronic infection or inflammation
Clinical Presentation
I) History (Symptoms)
Dyspnea on exertion – Most common presenting symptom
Fatigue and weakness – Due to decreased tissue perfusion
Palpitations – From tachycardia
Orthopnea, PND – If pulmonary congestion develops
Peripheral edema – From volume overload
Warm extremities – Classic sign, differentiates from low-output HF
Bounding pulses and wide pulse pressure
II) Physical Exam (Signs)
Vital Signs:
- Tachycardia
- Wide pulse pressure
- Elevated systolic BP, low or normal diastolic
- Warm, flushed extremities
- O2 saturation – Look for high venous oxygen content (from AV shunts)
Cardiovascular:
- S3 gallop
- Displaced apical impulse
- Jugular venous distension (JVD)
- Bounding peripheral pulses
Pulmonary:
- Rales or crackles if pulmonary congestion present
Abdomen:
- Hepatomegaly, possible ascites in cirrhosis
Peripheral:
- Edema, particularly in dependent areas
- AV bruit (in AV fistulas or shunts)
Differential Diagnosis (DDx)
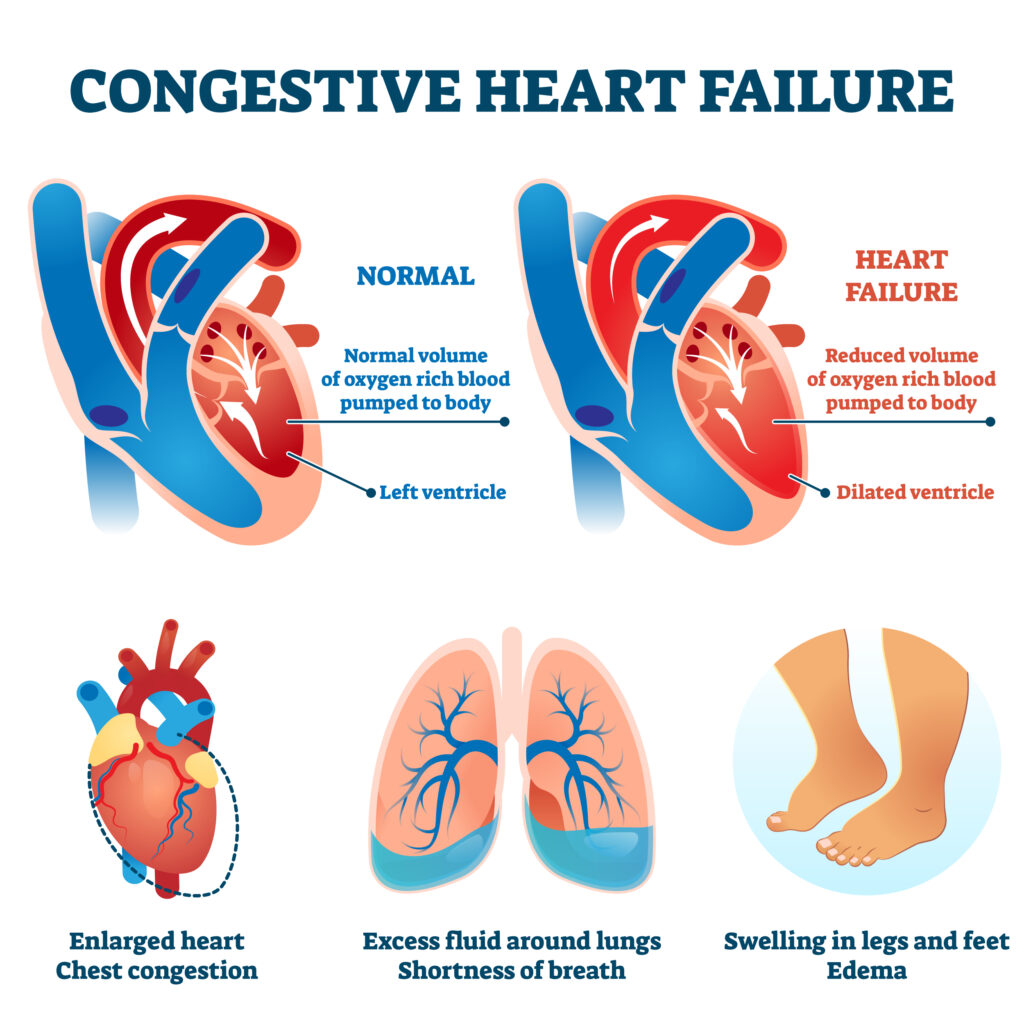
Low-output heart failure (HFrEF, HFpEF)
Thyrotoxic cardiomyopathy
Septic shock
Severe anemia without HF
Cirrhosis without cardiac involvement
Arteriovenous malformation
Beriberi (wet vs. dry)
Diagnostic Tests
Initial Tests
- Echocardiogram (Transthoracic) – Hyperdynamic LV function, EF >70%, elevated filling pressures
- EKG – Sinus tachycardia, possible LVH or signs of strain
- Chest X-ray – Cardiomegaly, pulmonary vascular congestion
Additional Tests
- Cardiac output measurement (via right heart catheter): Output >8 L/min
- Systemic vascular resistance (SVR) – Low (<800 dynes/sec/cm⁵)
Lab Tests
- CBC – To detect anemia
- TSH, Free T4 – Evaluate for thyrotoxicosis
- BNP/NT-proBNP – Often elevated
- CMP – Liver/kidney function
- Thiamine level – If beriberi suspected
- Lactate – To evaluate for hypoperfusion
- Arterial blood gases – May show metabolic acidosis
Treatment
I) Treat Underlying Cause
Anemia – Transfuse or treat underlying cause
Hyperthyroidism – Antithyroid drugs (methimazole, PTU), beta-blockers
AV fistula – Surgical correction or embolization
Beriberi – High-dose thiamine replacement
Cirrhosis – Optimize volume, consider liver transplant
Obesity – Weight loss and manage comorbidities
II) Symptomatic Treatment (if volume overload)
Diuretics – Loop diuretics (e.g., furosemide)
Beta-blockers – Reduce HR, improve filling time
Afterload reduction – Cautious use if hypertension present
Salt restriction and fluid restriction if significant edema
III) Avoid
Inotropes – Typically not indicated due to already high cardiac output
Excessive diuresis – May worsen perfusion if SVR is low
Consults
Cardiology – For diagnosis confirmation, echo/cath, and management
Endocrinology – If thyrotoxicosis or metabolic causes
Hematology – For anemia work-up
Nutritionist – Thiamine deficiency, weight loss strategies
Interventional radiology/surgery – For AV malformations
Patient Education
Educate on symptoms of worsening HF (weight gain, edema, fatigue)
Importance of treating underlying conditions (e.g., thyroid disease)
Avoid excessive salt or fluid intake
Encourage smoking cessation and healthy diet
Screen for alcohol use and nutritional deficiencies
Vaccines:
Annual influenza vaccine
Pneumococcal vaccine per age and risk group
COVID-19 vaccination as indicated
Follow-Up
Regular monitoring of symptoms, weight, and volume status
Periodic echocardiography
Re-evaluate for resolution of underlying cause
Close follow-up after initiation of treatment to prevent readmissions
Stay on top of medicine. Get connected. Crush the boards.
HMD is a beacon of medical education, committed to forging a global network of physicians, medical students, and allied healthcare professionals.