Cardiology > Pacemakers and Implantable Cardioverter-Defibrillators
Pacemakers and Implantable Cardioverter-Defibrillators (ICDs)
Background
Pacemakers are implantable devices that deliver timed electrical impulses to stimulate cardiac contraction when the intrinsic rhythm is too slow or conduction is impaired.
Implantable Cardioverter-Defibrillators (ICDs) are devices capable of both pacing and delivering high-energy shocks to terminate life-threatening ventricular arrhythmias such as ventricular tachycardia (VT) and ventricular fibrillation (VF).
Both devices are central to the management of conduction abnormalities and malignant arrhythmias. Pacemakers restore adequate heart rate and AV synchrony, while ICDs prevent sudden cardiac death by promptly detecting and treating ventricular arrhythmias.
Classification/Types
Pacemakers
Single-Chamber: Lead placed in right atrium or right ventricle.
Dual-Chamber: Leads in right atrium and right ventricle for AV synchrony.
Biventricular (Cardiac Resynchronization Therapy, CRT-P): Leads in right atrium, right ventricle, and coronary sinus for left ventricular pacing—used in heart failure with wide QRS.
ICDs
Single-Chamber ICD: Lead in right ventricle, detects and treats VT/VF.
Dual-Chamber ICD: Leads in right atrium and right ventricle, also provides atrial pacing if needed.
CRT-D: Combines resynchronization therapy with defibrillation for patients with advanced heart failure and arrhythmia risk.
Subcutaneous ICD (S-ICD): Implanted under skin without intracardiac leads, suitable for patients with high infection risk or challenging venous access.
Clinical Rationale
Bradyarrhythmias: Pacemakers prevent hemodynamic compromise from sinus node dysfunction or AV block.
Tachyarrhythmias: ICDs prevent sudden cardiac death by recognizing rapid ventricular rhythms and delivering pacing (anti-tachycardia pacing, ATP) or shocks.
Dyssynchrony: Biventricular pacing improves coordination of ventricular contraction, reducing morbidity in systolic heart failure.
Indications
Pacemakers
Symptomatic bradycardia due to sinus node dysfunction.
Advanced AV block (Mobitz II or complete heart block).
Chronotropic incompetence (failure to increase heart rate appropriately).
Biventricular pacing for HFrEF with LVEF ≤35% and QRS ≥120–150 ms.
ICDs
Secondary prevention: Survivors of cardiac arrest due to VT/VF not from reversible cause.
Secondary prevention: Sustained VT with hemodynamic compromise.
Primary prevention: Ischemic or non-ischemic cardiomyopathy with LVEF ≤35% and symptomatic heart failure despite optimal medical therapy.
Genetic arrhythmia syndromes (e.g., Brugada, long QT, hypertrophic cardiomyopathy with high sudden death risk).
Contraindications
Pacemaker: Asymptomatic bradycardia; reversible bradyarrhythmia (drug-induced, sleep-related).
ICD: Patients with limited life expectancy (<1 year) due to non-cardiac disease; recurrent VT/VF due to completely reversible causes.
Diagnostic Yield and Efficacy
Pacemakers improve symptoms, exercise tolerance, and quality of life in bradyarrhythmias.
CRT improves survival, reduces hospitalizations, and improves functional class in eligible heart failure patients.
ICDs reduce sudden cardiac death and all-cause mortality in both secondary and select primary prevention populations.
Procedure and Technique
Preparation: Anticoagulation review, venous access planning, sterile field preparation.
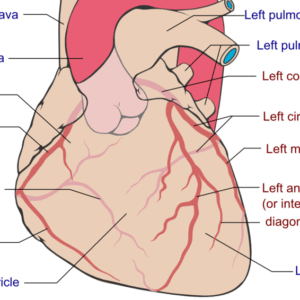
Implantation: Leads introduced via subclavian, axillary, or cephalic vein into right atrium, right ventricle, or coronary sinus. Device generator placed subcutaneously in infraclavicular pocket.
Programming: Tailored detection, pacing thresholds, and shock parameters.
Follow-up: Device interrogation in office or remotely to assess function, battery life, and stored arrhythmia data.
Physical Exam Findings Correlated
Vital Signs
Bradycardia or pauses (pacemaker indication).
Tachycardia, syncope, or sudden collapse (ICD indication).
General Appearance
Syncope, presyncope, or fatigue in bradyarrhythmias.
History of resuscitated cardiac arrest or heart failure exacerbations.
Cardiovascular System
Irregular or slow pulse.
Wide QRS with dyssynchrony in CRT candidates.
Neurological System
Syncope or seizure-like activity from transient cerebral hypoperfusion during arrhythmia.
Advantages
Pacemakers: Reliable symptomatic relief, restoration of heart rate, improved quality of life.
ICDs: Proven reduction in sudden cardiac death.
CRT: Mortality benefit and improved heart failure outcomes.
Remote monitoring enhances early detection of device or arrhythmia issues.
Limitations
Invasive implantation with procedural risks.
Battery life limited (5–10 years, requiring replacement).
ICD shocks can cause pain, anxiety, or inappropriate shocks.
Pacemakers and ICDs do not treat underlying structural heart disease.
Complications
Pocket hematoma or infection.
Lead dislodgement or fracture.
Venous thrombosis or occlusion.
Device malfunction or inappropriate shocks.
Rare: cardiac perforation, tamponade, pneumothorax.
Follow-Up and Clinical Decision-Making
Routine checks every 3–12 months or via remote telemetry.
Device interrogation to review arrhythmia episodes, pacing percentages, and lead function.
Anticoagulation decisions guided by atrial arrhythmia detection in pacemaker/ICD patients.
Reprogramming as patient’s rhythm or clinical condition evolves.
Stay on top of medicine. Get connected. Crush the boards.
HMD is a beacon of medical education, committed to forging a global network of physicians, medical students, and allied healthcare professionals.